Dermatologic Surgery 2000; 26(2): 160-162
The Logic of Follicular Unit Transplantation
Follicular Unit Transplantation is a method of hair restoration surgery where hair is transplanted exclusively in its naturally occurring, individual follicular units. Specifically, single strip harvesting, stereo-microscopic dissection, and large transplant sessions will be reviewed.
A donor is better if it is as small as possible. The reason is that if a donor is big, hairs grow in … a very unnatural appearance.
Hajime Tamura – 19431
Preservation of the Follicular Unit
The underlying premise of follicular unit transplantation is that the intact, individual follicular unit is sacred. Theoretically, they should neither be broken up into smaller units, nor combined into larger ones.2,3,4
This simple idea may not seem like a radical approach to hair transplantation, but when viewed in the context of how the surgery has been performed over the past forty years (when the very existence of the follicular unit went generally unrecognized), it is radical indeed. At present, the majority of hair transplant surgeons will, at times, combine several follicular units or split them up, as they are not convinced that this has a significant impact on either the anesthetic outcome or upon growth. Practitioners of follicular unit transplantation, however, are certain that only this procedure achieves the best cosmetic results and their hair “bristles” when they witness surgical techniques that divide follicular units or transect follicles, techniques they feel preclude optimal growth and waste precious donor hair. In spite of the heated debate, good scientific studies have not yet been performed to resolve these issues.
The follicular unit was first defined by Headington in his landmark 1984 paper “Transverse Microscopic Anatomy of the Human Scalp.5 The follicular unit includes:
1. 1 to 4 terminal follicles
2. 1, or rarely 2, vellus follicles
3. associated sebaceous lobules
4. insertions of the arrector pili muscles
5. perifollicular vascular plexus
6. perifollicular neural net
7. perifolliculum – cirumferential band of fine adventitial collagen that defines the unit
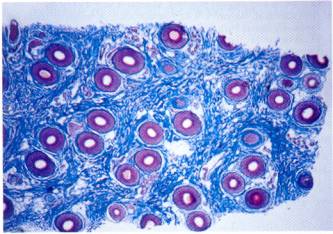
Photo: Follicular units at the level of the papillary dermis above the entry of the sebaceous duct. Each hexagonal follicular unit encloses sebaceous glands, sebaceous ducts, and several terminal and/or “vellus” hairs. Trichrome staining demonstrates pink keratin, smooth muscle, and blue collagen.
Photo courtesy of Dr. David Whiting
Transplanting Individual Follicular Units
That scalp hair grows in follicular units, rather than individually, is most easily observed by densitometry, a simple technique whereby scalp hair is clipped to approximately 1mm in length and then counted observed via magnification. What is strikingly obvious when one examines the scalp by this method, is that follicular units are relatively compact, and are surrounded by substantial amounts of non-hair bearing skin. The actual proportion of non-hair bearing skin is probably on the order of 50%, so that its inclusion in the dissection will have a substantial effect upon the outcome of the surgery. The great benefit of using individual follicular units is that the wound size can be kept to a minimum, while at the same time maximizing the amount of hair that can be transplaced.
Small Recipient Sites
The importance of minimizing the wound size in any surgical procedure cannot be over emphasized and hair transplantation is no exception. The effects of recipient wounding are felt at many levels. Large wounds can lacerate blood vessels and although the blood supply of the scalp is extensively collateralized, any damage to these vessels will have an impact on local tissue perfusion. An equally important issue is to minimize the disruption of the microcirculation. This is especially important when transplanting grafts in large quantities. The compact follicular unit is, of course, the ideal way to permit the use of the smallest possible recipient site, and has made the transplantation of large numbers of grafts technically feasible.
Densities between 10 to 40 follicular units per centimeter are routinely reported. Densities greater than 40 follicular units per centimeter in a single session have been accomplished, but may result in a decrease yield in some patients. It is important to note that a follicular unit density of 40 units/mm2 can create a hair density of over 120 hairs/mm2 (if all 3- and 4-hair units are used in select areas), and this is a density that many hair transplant surgeons feel is not necessary, or even desirable, to exceed.
Transplanting Follicular Units in Large Sessions
Putting aside anatomic, physiologic and technical issues for the moment, it is important to emphasize the practical reasons to strive toward large sessions. The specific events that bring a balding patient to the doctor for hair loss will vary, but the common denominator of those seeking hair restoration is to improve their appearance, and to improve the quality of their life, be it personal, professional, or social.
Until the transplant is cosmetically acceptable, the disruptions from the scheduling of multiple surgeries, the limitations in activity, and the concern about their discovery, can place a patient’s life “on hold.” It should therefore be incumbent upon the physician to accomplish their objectives as quickly as possible. Some patients prefer smaller sessions for economic reasons.
Microscopic Dissection
There is probably no other aspect of follicular unit transplantation that has generated more controversy than the use of the microscope. Stereo-microscopic dissection was introduced into the field of hair transplantation by Dr. Bobby Limmer6 in 1987.
The following statements summarize the use of magnification:
- In order to dissect intact individual follicular units, you must be able to see them clearly.
- Only magnification allows their clear visualization in both normal and scarred skin, independent of the specific hair characteristics of color, hair shaft diameter, and curl.
Follicular dissection can logically be divided into two parts; the subdivision of the initial donor strip into smaller pieces and the further dissection of these pieces into individual follicular units. The first part of the procedure, the handling of the intact strip, has always been the most problematic. The intact strip however, is difficult to stabilize and is too opaque for transillumination to be useful.
The dissecting microscope and other magnification methods allow the strip to be divided into sections (or “slivers”) by actually going around follicular units leaving them intact. The dissecting stereo-microscope is able to accomplish this because of its high resolution (usually 5x more powerful than magnifying loops) and its intense halogen top-lighting that provides continuous illumination, as one dissects through the strip. Back light illumination has also proven beneficial. Stability can easily be achieved by applying slight traction to the free end of the strip. The thin slivers are then laid on their sides and the microscopic dissection of the individual units is completed. With stereo-microscopic dissection, except for the outer edges of the ellipse, every aspect of the procedure is performed under direct visualization, so that follicular transection can be minimized and the follicular units maintained.
Conclusion
The entire field of hair restoration surgery has moved toward the use of follicular unit transplantation. While the exclusive use of follicular units is not employed by the majority of transplant surgeons,. The impact of this approach has been significant. Hair restoration surgeons are becoming more scientific and precise in their approach to this field. The vague terminology of the past, i.e., round grafts, many grafts, micro grafts, has been replaced with more precise terms. We now converse in a language which details the number of follicular units per square centimeter, hair shaft diameter in microns, and incisional density of the recipient site for any given session. Perhaps the modern era of transplantation did not begin with the micrografting of the ’80’s, but its is only truly being realized with follicular Unit transplantation of the ’90’s.
References
- Tamura: Hair grafting procedure, JPN J Dermatol Venereol [Japanese] 52(2):1943.
- Bernstein RM, Rassman WR, Szaniawski W, Halperin A: Follicular Transplantation.
International Journal of Aesthetic an Restorative Surgery 3:119-132, 1995. - Bernstein RM, Rassman WR: Follicular Transplantation: Patient Evaluation and Surgical Planning.
Dermatologic Surgery 23:771-784, 1997. - Bernstein RM, Rassman WR: The Aesthetics of Follicular Transplantation. Dermatologic Surgery 23:785-799, 1997.
- Headington JT: Transverse Microscopic of the Human Scalp. Archives of Dermatology 120:449-456, 1984.
- Limmer BL: Elliptical Donor Stereoscopically Assisted Micrografting as an Approach to Further Refinement in Hair Transplantation. Dermatologic Surgery 20:789-793, 1994.